The Placenta & Twinning
Professor A. Cuschieri
Department of
Anatomy
University of Malta
Objectives:
o
Name the structures that form the placenta
o
Distinguish between the foetal and maternal contributions to the
placenta
o
List the main functions of the placenta
o
Distinguish between identical and fraternal twins and how they arise
o
Explain how identical twins can share a common amnion and chorion
Introduction
When the
blastocyst embeds itself in the maternal endometrium it is covered with
chorionic villi derived from the syncitiotrophoblast and cytotrophoblast. The
distribution and size of the villi are not uniform throughout the surface of
the chorion.
The chorion frondosum
consists of numerous villi over the embryonic pole. This will contribute to the
formation of the placenta .
The chorion laeve contains very
sparse villi over the abembryonic pole. The villi will eventually disappear,
and here the chorionic membranes are formed.
The
Placenta is derived from two sources:
• The foetal chorion
• The maternal deciduas
By the third week tertiary chorionic villi are formed.
New chorionic villi continue to
sprout out at different gestational ages
At 9 -16 weeks they are termed mesenchymal villi
At 16 -25 weeks they are
immature intermediate villi. At this
age the cytotrophoblast persist only in patches.
At 25-32 weeks they form mature
intermediate villi.
After 32 weeks they sprout out
terminal villi (consisting of a thin
syncitiotrophoblast and foetal capillaries with minimal intervening mesoderm)
The Placenta
consists of branched chorionic villi bathed in lacunae of maternal blood.
On the foetal surface of the
placenta the chorion forms a continuous surface from which the villi
arise. The cytotrophoblast proliferates
from the tips of the villi and forms a cytotrophoblastic shell on the maternal
surface of the placenta. Elsewhere the
villi are lined by syncitiotrophoblast, while the cytotrophoblast becomes
restricted to small patches.
The Decidua
The decidua is derived from the
secretory endometrium, which continues to proliferate and secrete under the
influence of persistent high levels of progesterone, which in turn is
stimulated by increasing levels of HCG, secreted by the growing
syncitiotrophoblast. As the decidual
cells continue to proliferate, they
accumulate lipids and glycogen, and, the whole decidua becomes more vascular.
Septa grow from the decidua and
project into the intervillous spaces dividing the placenta into 15 to 20 cotyledons.
At 4 weeks (2nd
month) the amniotic cavity grows and obliterates the chorionic cavity
(extra-embryonic coelom).
The amnion fuses with the
chorion to form the chorio-amniotic plate.
The placenta at birth:
o
Is 15 to 25 cm in diameter
o
Consists of 15 to 20 cotyledons
o
Weighs 500 to 600 grams
o
Is supplied by 80 to 100 spiral arteries
Functions of the placenta
1.
Exchange of gases mainly by
diffusion
2.
Exchange of metabolites:
a. Carbohydrates
b. Amino acids
c. Fatty acids
d. Vitamins
e. Electrolytes
Waste products: urea, creatinine, bilirubin etc
3.
Transport of maternal
substances:
a.
Maternal
antibodies IgG conveys passive immunity to the new-born infant
b.
Transferrin
- for iron transport
c.
Maternal
hormones - may affect foetus
d.
Chemical,
drugs, viruses - all potentially teratogenic
4.
Secretion of hormones - into maternal circulation:
a.
Human
chorionic gonadotrophin
b.
Progesterone
and oestrogen
c.
Somato-mammotropin
Passage of cells into the maternal circulation. This is acquiring increasing importance because new methods are being developed to isolate the foetal cells from the maternal blood, and use them for prenatal diagnosis instead of the invasive methods of amniocentesis and chorionic villus biopsy.
The
umbilical cord consists of:
o
Two umbilical arteries
o
One umbilical vein
o
Wharton’s jelly
o
And, only its most proximal
part,
o
The yolk sac and
vitello-intestinal duct
o
The allantoic diverticulum
o
A canal connecting the
extra-and intra-embryonic coeloms, which is subsequently obliterated.
The amniotic
fluid
o
800 – 1000 ml
o
functions as a “shock
absorber” for the foetus
o
Allows foetal movements
o
Is replaced every 3 hours
o
Circulates
continuosly:
o
It is ingested through
mouth
o
Excreted as urine
Abnormalities of amniotic fluid
1.
Oligohydramnios
- Usually occurs with renal agenesis
- Causes foetal compression syndrome (Potter’s syndrome)
2. Polyhydramnios
- Usually occurs with oesophageal atresia
Twinning
There are two types of twins:
a.
Fraternal twins are the result of fertilization of two oocytes. The two zygotes develop and implant
themselves separately. They have
separate placentae and amniotic cavities.
Like all sibs born to the same couple, they have half their genes in
common. They may be of different sex or
of the same sex.
b.
Identical twins are derived from a single zygote, which during early
development divides into two groups of cells that continue to develop
independently. Identical twins are
always of the same sex, and have identical genes. Identical twins are in fact clones as the two individuals are
derived from the same cell.
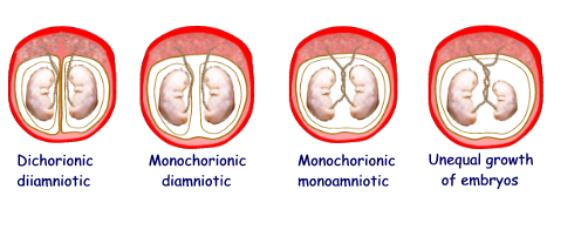
Identical twins may share the
same placenta or amniotic cavity, or they may have different placentae and
amniotic cavities, depending on the developmental stage at which the separation
of the conceptus into two twins occurs:
 1. Separation of the blastomeres
1. Separation of the blastomeres
into two groups which develop and implant separately. They result in
two separate placentae and gestational sacs (dichorionic,
diamniotic)
 2. Separation of the inner cell mass or embryoblast into two groups
forms two amniotic cavities but one chorion and placenta (form monochorionic,
diamniotic twins)
2. Separation of the inner cell mass or embryoblast into two groups
forms two amniotic cavities but one chorion and placenta (form monochorionic,
diamniotic twins)
3. Separation of the bilaminar disc into two groups of pluripotent cells forms two embryos sharing a single amniotic cavity, chorion and placenta (form monamniotic, monochorionic twins)
4.
Incomplete separation of the inner cell mass gives rise
to conjoined twins.
5.
Anastomosis between the circulations of monoamniotic twins may cause failure
of normal growth and development in one embryo