Preparation For Pregnancy
Professor Alfred Cuschieri
Department of Anatomy, University of Malta
Objectives:
o Distinguish between FSH, LH and chorionic gonadotrophin, and where they are synthesised
o Distinguish between primordial, primary and secondary follicles
o Name the functions of the granulosa cells and the theca folliculi
o Describe the structure of the oocyte immediately after ovulation
o Name the functions of oestrogen and progesterone
o Correlate hormonal changes with the phases of the menstrual cycle
o State how the endometrium is affected by a pregnancy
o Outline the mechanisms of action of substances that inhibit and others that stimulate ovulation or spermatogenesis.
o Explain the hormonal changes in post-menopausal
Cyclic Changes In The Female Genital System
The female genital system undergoes a series of cyclic interdependent changes that bring about ovulation and prepare the genital tract for an eventual pregnancy. If pregnancy does not ensue a new cycle commences at approximately monthly intervals. These changes affect
1. The development of the oocyte and ovarian follicle, culminating in ovulation and the formation of a corpus luteum (The ovarian cycle)
2. The uterine endometrium culminating in menstruation if pregnancy does not ensue (The menstrual cycle)
3. A series of hormonal changes that control the cycle:
a. Gonadotrophin releasing hormone (GnRH), released by the hypothalamus and acting on the gonadotrophs of the anterior pituitary.
b. Follicle Stimulating Hormone (FSH), and Luteinising Hormone (LH) secreted by the gonadotrophs of the anterior pituitary. These hormones are called gonadtrophins because they act on the gonads and bring about the changes in the ovarian cycle
c. Oestrogen and progesterone, secreted by the ovarian follicular cells and corpus luteum respectively act on the endometrium stimulating the cyclical changes of the menstrual cycle.
All these cyclical changes are inter-related and inter-dependent. The cycle begins when all the hormones are at their lowest levels and the development of primary follicles while the endometrium commences menstruation. For practical purposes day 0 of the cycles corresponds to the first day of menstruation.
The cyclical changes are divided into 3 phases as follows:
1. The Oestrogen phase extends from day 0 to the time of ovulation, approximately on day 14. The oocyte and follicles undergo the following changes:
a. Primordial follicles (Days 0 to 3). These consist of a primary oocyte surrounded by a layer of flattened follicular cells. The oocyte is in the diplotene stage of meiosis I, and in meiotic arrest at this stage since foetal life. A rise in GnRH stimulates a gradual rise in the level of FSH. This in turn stimulates 5 to 20 primordial follicles to begin to develop.
b. Primary follicles (Days 3 to 8). These consist of a primary oocyte surrounded by a layer of cubical follicular cells. The oocyte is covered by a number of micovilli, and the follicular cells have processes that contact the oocyte plasma membrane and have gap junctions between them.
c. Secondary follicles (Days 8 to 10). The oocyte influences the granulosa cells to proliferate and organize the development of a secondary follicle
i. The follicular cells proliferate and become multilayered – they may also be called granulosa cells, which secrete oestrogens The granulosa cells are stimulated to proliferate by the action of activin, a signaling protein that is a member of the family of transforming growth factor-b (TGF-b), which is released by the oocyte. FSH also acts on the granulosa cells, and enhances the action of activin. The granulosa cells secrete Meiosis inhibiting factor (MIF).
ii. A follicular antrum forms by accumulation of fluid between the follicular cells
iii. A zona pellucida forms around the primary oocyte. This consists of glycoprotein and glycosaminoglycans. It is secreted jointly by the oocyte and the follicular cells. The processes between the follicular cells and the oocyte are maintained through the zona pellucida.
iv. The theca folliculi is derived from the ovarian stroma surrounding the follicle and consists of
- a theca interna, which is cellular and secretes androgens, which are then converted to oestrogen by the granulosa cells
- a theca externa, which is fibrous.
v. Although many follicles begin to develop, only one usually becomes dominant, while the rest degenerate
d. Graafian follicle (Days 11 to 14).
i. The antrum containing liquor folliculi enlarges until it is about 2 cm in diameter
ii. The cumulus oophorus is a mass of follicular cells that surround the oocyte and projects into the antrum
iii. The membrana granulosa is the layer of follicular cells that surrounds the antrum
iv. A surge of LH occurs at mid-cycle (day 14) stimulates:
- Production of maturation-promoting factor
- Release of the oocyte from meiotic arrest
- Withdrawal of processes and gap junctions of the follicular cells
- Withdrawal of the oocyte microvilli, forming a perivitelline space
- Completion of the first meiotic division to form a secondary oocyte
- Extrusion of the first polar body
- Secretion of progesterone by the granulosa and theca interna
- The Graafian follicle to point and bulge on the surface of the ovary
-
2. Ovulation occurs when the Graafian follicle ruptures, releasing the oocyte.
At the time of  ovulation the oocyte
ovulation the oocyte
- is a secondary oocyte
- is surrounded by a zona pellucida
- is surrounded by the corona radiata
- has a polar body within the zona pellucida
3. The Progesterone or Luteal phase extends from the time of ovulation to the end of the cycle (Days 14 to 28)
a. The membrana granulosa of the collapsed Graafian follicle proliferates forming a corpus luteum
b. They undergo the lutein reaction converting them into steroid secreting cells secreting progesterone in increasing levels as the crpus luteum grows
c. The corpus luteum becomes vascularized by growth of blood vessels from the theca interna
d. Proliferation of fibroblasts from the theca externa form connective tissue trabeculae within the corpus luteum
The Menstrual Cycle
 The stages of the menstrual cycle are consequent on the ovarian
cycle and the hormonal changes. They
are divided into 3 phases:
The stages of the menstrual cycle are consequent on the ovarian
cycle and the hormonal changes. They
are divided into 3 phases:
1. The menstrual and recovery phase corresponds to the first three days of the ovarian cycle when the hormones are at their lowest levels and the primordial follicles are being stimulated to develop. The endometrium consists of the basal layer of endometrial stroma, the basal parts of the glands and the basal stumps of blood vessels. Following shedding of the epithelium as a result of ischaemia, the surface epithelium is regenerated from the epithelium lining the basal parts of the glands.
2. The oestrogen or proliferative phase. Increasing levels of oestrogen secreted by the granulosa cells of the secondary follicle stimulates proliferation of the endometrium. The proliferative endometrium consists of:
a. A columnar epithelium
b. Tubular glands
c. A cellular endometrial stroma
d. Proliferating blood vessels
3. The progesterone or secretory phase. Following ovulation, secretion of progesterone by the corpus luteum stimulates the endometrium to become secretory, oedematous and highly vascular. The proliferative endometrium is characterised by
a. Distended and secretory glands that have a serrated outline.
b. An oedematous stroma containing extracellular fluid.
c. Large, tortuous blood vessels.
The endometrium at this stage has all the necessary characteristics to receive a developing embryo.
If fertilization occurs:
-
the
oocyte completes the second meiotic division
-
the
zygote develops into a conceptus
-
implantation
occurs 5-6 days after fertilization
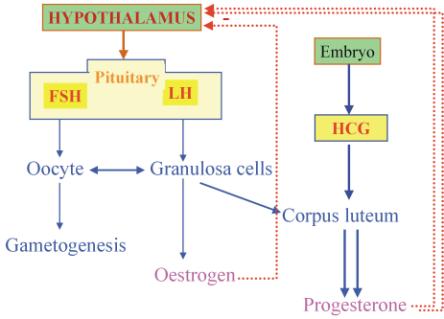
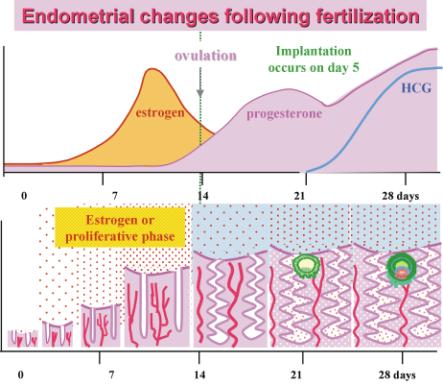 Following implantation, the
conceptus secretes Human Chorionic Gonadotrophin (HCG), which is very similar
to LH and has similar effects. This
causes the corpus luteum to continue to proliferate and to secrete increasing
levels of progesterone so that the secretory endometrium is maintained.
Following implantation, the
conceptus secretes Human Chorionic Gonadotrophin (HCG), which is very similar
to LH and has similar effects. This
causes the corpus luteum to continue to proliferate and to secrete increasing
levels of progesterone so that the secretory endometrium is maintained.
If fertilization does not occur, the secondary oocyte degenerates, HCG is not produced, the level of progesterone falls, causing constriction of the endometrial blood vessels, ischaemia of the endometrium, which is therefore not maintained and menstruation occurs.
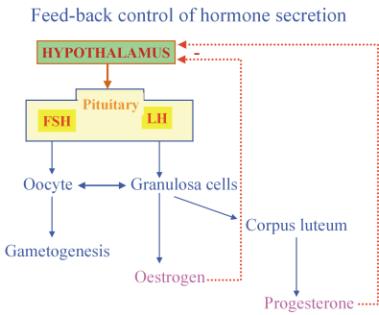
Feed-back control of Hormone secretion
The levels of circulating hormones are regulated by a fee-back mechanism. Increased levels of circulating oestrogen and progesterone have in inhibitory effect on the hypothalamic neurons, whcich through GnRH decrease the secretion of FSH and LH.
Menarche is the onset of the menstrual cycle. It occurs at the age of about 12 years. There is minimal FSH and LH stimulation in pre-pubertal children.
Menopause is the cessation of the menstrual cycle. It occurs at the age of 38-48 years. In post-menopausal women the supply of primordial follicles has been completely exhausted. There are very low levels of estrogen and progesterone, and the hypothalamus responds by secretion of more FSH to stimulate oogenesis. Post-menopausal women have very high FSH but low estrogen and progesterone. This may cause several symptoms including hot flushes, excessive sweating, night sweats, headache, changes in mood, changes in concentration, vaginal dryness and altered sexual desire, insomnia, and osteoporosis. These symptoms may be prevented by hormone replacement therapy (HRT), by controlled doses of oestrogen and progesterone to mimic the menstrual cycle. These may be administered by the use of skin patches that release oestrogens and progesterone, which are absorbed transcutaneously.
During pregnancy there are high levels of human chorionic gonadotrophins (HCG) secreted by the embryonic trophoblast. HCG is very similar to LH, stimulates the corpus luteus to enlarge and secrete more progesterone. The negative feed-back on the hypothalamus inhibits further ovulation, but the sustained secretion of progesterone is maintained by the future placenta.
Contraception by Hormones
Administration of cyclical doses of oestrogen and progesterone with relatively high doses of oestrogen on the first day of menstruation sets up a feed-back inhibition on the hypothalamus, which inhibits secretion of FSH, thus inhibiting follicular development.
Stimulation of ovulation
Clomiphene citrate is a non-steroidal anti-oestrogen. This suppresses the feed-back inhibition by oestrogen, and stimulates the release of FSH and LH. stimulates
Clinical use of FSH and LH
FSH is isolated from the urine of menopausal women and is known as Human Menopausal Gonadotrophin (HMG). HMG is used clinically to stimulate ovulation and to stimulate spermatogenesis. It’s effect is more rapid than that of clomiphene. It is used to stimulate ovulation prior to assisted fertilization.
Two Important Changes Occur in Women at the Time of Ovulation
1. Qualitative change in the vaginal secretions, which are in fact derived from the cervical glands. They become very viscous and sticky and can be pulled into strands.
2. Slight rise in body temperature
Both these phenomena are sometimes used as indicators of the time of ovulation, and may be used to determine the “safe period”. In some women these changes are not prominent enough for accurate determination of the time of ovulation.
Human Chorionic Gonadotrophin (HCG) is obtained from the urine of pregnant women. It is similar to
LH. HCG is used clinically to stimulate
the interstitial cells to secrete
androgen in males and thus to stimulate development of male secondary
sex characteristics.
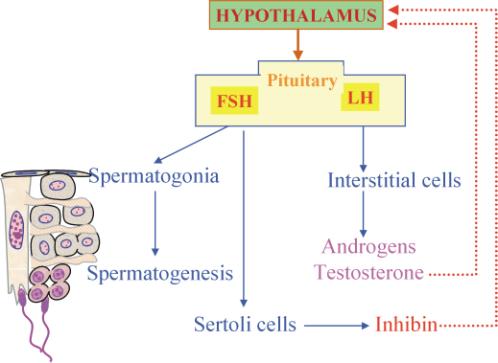
Hormone Feed-Back In Men
A similar feed-back mechanism also applies in males, as illustrated in the following diagram. LH acts on the interstitial cells of Leidig, stimulating them to produce testosterone and other androgen hormones, which exert a negative feedback on the hypothalamus and decreased LH secretion. FSH stimulates spermatogenesis, and the Sertoli cells, which in turn produce inhibin that inhibits the hypothalamus.
Semen
Semen consists of spermatozoa produced in
the seminiferous tubules, and secretions
from the prostate gland and the seminal vesicles. A normal ejaculate has a volume of 2-6 ml, and contains 50 to 150 million
spermatozoa per ml. About 10% of the
spermatozoa have an abnormal morphology, involving the head, tail or mid-piece.
The s
eminal vesicle secretions contain:
- fructose - for nutrition of spermatozoa
- mucoproteins - coagulate semen
- prostaglandins - induce contractions in female genital tract
The prostatic secretions contain:
- acid phosphatase
- fibrinolysin – liquefies the coagulated semen
- proteolytic enzymes
*************************